Our overall aim is to improve the diagnosis, treatment and understanding of brain tumours in children and young people. We have a number of projects covering a range of areas.
Imaging of Tumours Study CNS 2004 10:
The Imaging of Tumours Study is a single arm observational study (REC 04/MRE04/4; IRAS 32486) currently sponsored by the University of Birmingham. As of 2024, there are approximately 1800 patients recruited to the study from 11 centres in the UK.
The study originally opened in Oct 2004 as the MRS of Brain Tumours study, and the scope was widened in terms of imaging and tumour type in February 2012 when its name was updated to the Functional Imaging of Tumours Study. At that time, and within the patient information sheets, Functional Imaging, referred to imaging that gave more information than both size and site of tumour. Over time, this term has been interpreted differently and has begun to cause some confusion. As radiomics approaches have been developed such “functional” information can also increasingly be gained from standard imaging. Following a meeting of clinicians and scientists involved in the project, in Protocol Version 8.0, the title has been updated to the Imaging of Tumours Study and the term “functional” removed from the aims and specific areas of the protocol, and/or where appropriate replaced with terms for specific techniques (e.g. MR Spectroscopy (MRS).
In 2023, as Professor Andrew Peet retired and became Emeritus Professor, Dr John Apps took over as Chief Investigator, supported by Professor Peet, with a specific study management group (SMG) for this study. This is compiled of individuals with expertise across Radiology, Imaging Science, Pathology, Data Science, Medical Physics, and also working closely with patients and patient organisations to support the management of the study. The study has been closely linked to the Children’s Cancer and Leukaemia Group (CCLG) now called The Children & Young People’s Cancer Association, and closely integrated with the CCLG Functional Imaging Group. This close relationship will continue and the SMG will continue to work closely with the CCLG Functional Imaging Group, which itself is likely to update its name in the near future.
The data collected within this project has and is used for a range of subprojects focussed on specific aims within the overall objectives.
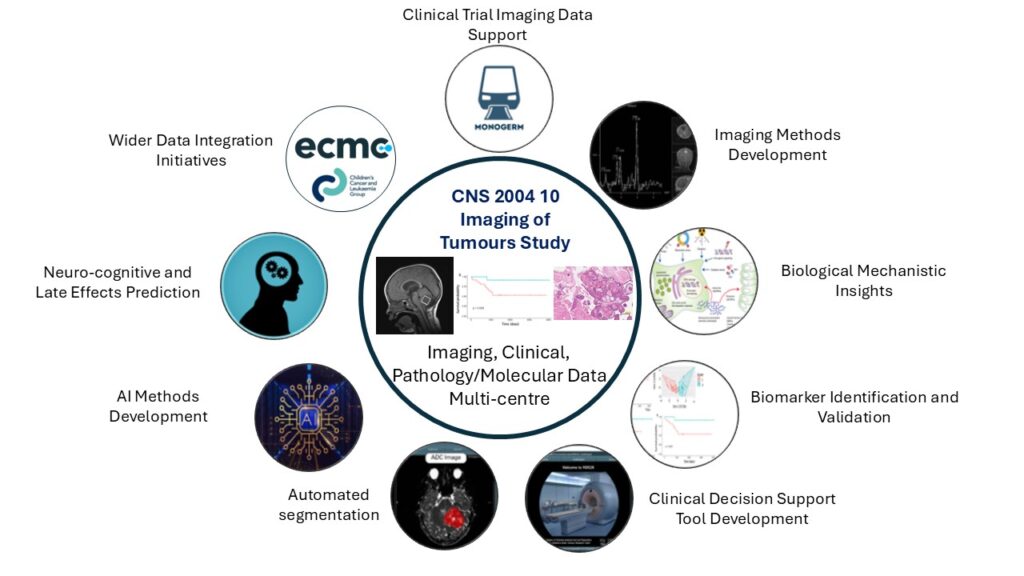
The range of subprojects include:
- Clinical Trial Imaging Data Support
- Imaging Methods Development
- Biological Mechanical Insights
- Biomarker Identification and Validation
- Clinical Decision Making Tool Development
- Automated segmentation
- AI Methods Development
- Neuro-cognitive and Late Effects Prediction
- Wider Data Integration Initiatives
Study aims
To develop imaging methods for the diagnosis, management and understanding of tumours in the fetus, children and young people.
To integrate analysis of imaging data, with clinical data and biological data for the improved understanding and characterisation and to support the diagnosis, treatment and monitoring of children with tumours.History
In the 1990s, considerable interest had developed around a set of imaging techniques which could probe tumour properties, called functional imaging. One of these, magnetic resonance spectroscopy could provide metabolite profiles of tumours and became a focus for two academic oncologists, Andrew Peet and Richard Grundy, who thought that magnetic resonance spectroscopy and tumour molecular genetics could improve not only our understanding of tumour metabolism but brain tumour characterisation in general. Following some earlier successes, there was also an intent to use computerised pattern recognition for the analysis, the beginnings of Artificial Intelligence. Initially funded by a local charity, the study was set up as a single centre study in Birmingham where they were both based. The hospital did not have an image storage PACS system then and a specific grant was awarded to set up a digitalised web accessible database which was set up by Kal Natarajan, a clinical scientist in computing. Substantial funding came from the Department of Health in 2002, and with the support of the Children’s Cancer and Leukaemia Group (then the UKCCSG and acting as a Clinical Trials Unit), the project became multi-centre. A new web accessible database was developed with Professor Theo Arvanitis, Engineering at University of Birmingham.
We were well supported by key figures at the major centres in the UK and the first patient was recruited by oncologist Darren Hargrave, then at the Royal Marsden Hospital, who has continued to be a strong supporter. We soon became partners in the EU Framework 6 Project eTumour which had similar objectives across the whole age range and provided an early example of data sharing between projects. Input from physicists has always been essential to this venture and the funding allowed recruitment of Nigel Davies and the first PhD student, Martin Wilson.
Increasing success led to the award of a Cancer Imaging Programme Grant by Cancer Research UK, EPSRC, MRC and NIHR. Study co-ordination became increasingly important and Jane Crouch undertook this from Birmingham, which had become the sponsor. Over the years, the study has broadened in scope for imaging types and tumour locations but is still faithful to the initial concept of probing childhood tumour properties with imaging and linking these with tumour biology. The projects supported by the study have been funded by most of the major funding bodies and many smaller charities. A large number of papers have been published ranging from technical advances to clinical studies of added value. The findings have been presented throughout the world and are increasingly being incorporated into a clinical decision support tool.
Recent and Significant Outputs
Primary Research papers
T. Zhao, J. T. Grist, D. P. Auer, S. Avula, S. Bailey, N. P. Davies, R. G. Grundy, O. Khan, L. MacPherson, P. S. Morgan, B. Pizer, H. E. L Rose, Y. Sun, M. Wilson, L. Worthington, T. N. Arvanitis, and A. C. Peet, Noise Suppression of Proton Magnetic Resonance Spectroscopy Improves Paediatric Brain Tumour Classification, NMR in Biomedicine, 37(6): e5129, 2024
S. K. Gill, H. E. L. Rose, M. Wilson, D. Rodriguez Gutierrez, L. Worthington, N. P. Davies, L. MacPherson, D. R. Hargrave, D. E. Saunders, C. A. Clark, G. S. Payne, M. O. Leach, F. A. Howe, D. P. Auer, T. Jaspan, P.S. Morgan, R. G. Grundy, S. Avula, B. Pizer, T. N. Arvanitis, and A. C. Peet, Characterisation of Paediatric Brain Tumours by their MRS Metabolite Profiles, NMR in Biomedicine, 37(5): e5101, 2024
S. Kohe, C. Bennett, F. Burté, M. Adiamah, H. Rose, L. Worthington, F. Scerif, L. MacPherson, S. Gill, D. Hicks, E. C. Schwalbe, S. Crosier, L. Storer, A. Lourdusamy, D. Mitra, P. S. Morgan, R. A. Dineen, S. Avula, B. Pizer, M. Wilson, N. Davies, D. Tennant, S. Bailey, D. Williamson, T. N. Arvanitis, R.G. Grundy, S.C. Clifford and A. C. Peet, Metabolite Profiles of Medulloblastoma for Rapid and Non-Invasive Detection of Molecular Disease Groups, EBioMedicine, 100:104958, 2024.
See this research explained in the following video.
Further publications
Apps, JR , Gonzalez-Meljem JM, Guiho R, Pickles JC, Prince E, Schwalbe E, Joshi N, Stone TJ, Ogunbiyi O, Chalker J, ABassey A, Otto G, Davies R, Hughes D, Brandner S, Tan E, Lee L, Hayhurst C, Kline C, Castellano S, Hankinson T, Deutschbein T,. Jacques TS & Martinez-Barbera JP. Recurrent adamantinomatous craniopharyngiomas show MAPK pathway activation, clonal evolution and rare TP53-loss-mediated malignant progression.Acta Neuropathologica Communications (2024) 12(127) https://doi.org/10.1186/s40478-024-01838-4
Apps JR , Maycock S, Ellison DW, Jaspan T, Ritzmann TA, Macarthur D, Malluci C, Wheatley K, Veal GJ, Grundy RG, Picton S, Phase II Study of Intravenous Etoposide in Patients with Relapsed Ependymoma (CNS 2001 04), Neuro-Oncology Advances, 2022, 13;4(1):vdac053. doi: 10.1093/noajnl/vdac053.
D. Zhao, J. T. Grist, H. E. L. Rose, N. P. Davies, M. Wilson, L. MacPherson, L. J. Abernethy, S. Avula, B. Pizer, D. R. Gutierrez, T. Jaspan, P. S. Morgan, D. Mitra, S. Bailey, V. Sawlani, T. N. Arvanitis, Y. Sun and A. C. Peet, Metabolite Selection for Machine Learning in Childhood Brain Tumour Classification, NMR in Biomedicine, e4673, 2022.
S. B. Withey, L. MacPherson, A. Oates, S. Powell, J. Novak, L. Abernethy, B. Pizer, R. Grundy, P. S. Morgan, S. Bailey, D. Mitra, T. N. Arvanitis, D. P. Auer, S. Avula and A. C. Peet, Dynamic Susceptibility-Contrast Magnetic Resonance Imaging with Contrast Agent Leakage Correction Aids in Predicting Grade in Pediatric Brain Tumours: A multicenter study, Pediatric Radiology, 10.1007/s00247-021-05266-7: 1-19, 2022
Apps JR, Stache C, Gonzalez-Meljem JM, Gutteridge A, Chalker J, Jacques TS, Forshew T, Holsken A, Martinez-Barbera JP, CTNNB1 mutations are clonal in adamantinomatous craniopharyngioma, Neuropathology and Applied Neurobiology, 2020, 46, 510-514
Apps JR, Carreno G, Gonzalez-Meljem JM, Haston S, Guiho R, Cooper JE, Manshaei S, Jani N, Hölsken A, Pettorini B, Beynon RJ, Simpson DM, Fraser HC, Hong Y, Hallang S, Stone TJ, Virasami A, Donson AM, Jones D, Aquilina K, Spoudeas H, Joshi AR, Grundy R, Storer LCD, Korbonits M, Hilton DA, Tossell K, Thavaraj S, Ungless MA, Gil J, Buslei R, Hankinson T, Hargrave D, Goding C, Andoniadou CL Brogan P, Jacques T, Williams HJ, Martinez-Barbera JP, Tumour compartment transcriptomics demonstrates the activation of inflammatory and odontogenic programmes in human adamantinomatous craniopharyngioma and identifies the MAPK/ERK pathway as a novel therapeutic target, Acta Neuropathol. 2018 135(5):757-777
Cresswell G*, Apps JR*, Chagtai T, Mifsud B, Bentley CC, M Mascietto, SD Popov, M Weeks, OE Olsen, NJ Sebire, K Pritchard-Jones, NM Luscombe, RD Williams, W Mifsud, Intra-tumour genetic heterogeneity in Wilms’ tumour: clonal evolution and clinical implication. EBiomedicine, 2016, 9, 120-9
Funding
The Imaging of Tumours study has been and continues to be supported by funding from a range of sources, including: Cancer Research UK and EPSRC Cancer Imaging Programme at the Children’s Cancer and Leukaemia Group (CCLG) in association with the MRC and Department of Health (England), Grant/Award Numbers: C7809/A10342; European Framework VI Grant eTUMOUR, Grant/Award Number FP6-2002-LIFESCIHEALTH 503094; EU Framework 6 STREP, Grant/Award Number IST-2004-2721; Department of Health National Clinician Scientist Award; NIHR Research Professorship, Grant/Award Numbers: NIHR-RP-R2-12-019; Cancer Research UK and NIHR Experimental Cancer Medicine Centre Paediatric Network, Grant/Award Numbers: C8232/A25261; Birmingham Women’s and Children’s Hospital Charities, Grant/Award Numbers BCHRF 065, 287, 316, 353, 513; The Children’s Cancer and Leukaemia Group Little Princess Trust, Grant/Award Numbers: 2017/15 and 2019/01; Children with Cancer, Grant/Award Numbers: 15/118; Action Medical Research and the Brain Tumour Charity, Grant/Award Numbers: GN2181; Health Data Research UK (HDR UK); Children’s Research Fund; Help Harry Help Others.
Get involved
Patients and Public: We are always happy to engage with patients and public about our research for more information please see the Get involved page.
Researchers: If you are interested in becoming involved in this project please contact the team at: [email protected]